Electronic Health Record Integration: The Complete Guide to Seamless Healthcare Data Connectivity in 2025
Electronic health record integration is transforming healthcare by enabling seamless data flow between disparate systems, improving patient outcomes, and driving significant cost savings. With 96% of hospitals having adopted certified EHR technology but only 30% achieving full interoperability Electronic Health Records Market Size, Share, Trends Report [2035], the opportunity for organizations to gain competitive advantage through strategic EHR system integration is enormous. Healthcare organizations implementing comprehensive integration strategies see 25% average revenue increases and potential annual savings of $25-30 billion across the U.S. healthcare system through improved interoperability.
Introduction: Healthcare’s Digital Transformation Imperative
In today’s rapidly evolving healthcare landscape, the average hospital generates approximately 50 petabytes of data annually, with healthcare data volume increasing at 47% per year EHRs: The Challenge of Making Electronic Data Usable and Interoperable – PMC. This explosive growth in health information has created both unprecedented opportunities and significant challenges for healthcare organizations worldwide.
Electronic health record integration has emerged as the critical foundation for managing this complexity, enabling healthcare providers to deliver superior patient outcomes while achieving operational excellence and financial sustainability. This transformation is part of broader healthcare digital transformation consulting initiatives that modernize healthcare delivery across all touchpoints.
Understanding Electronic Health Record Integration
What is EHR Integration?
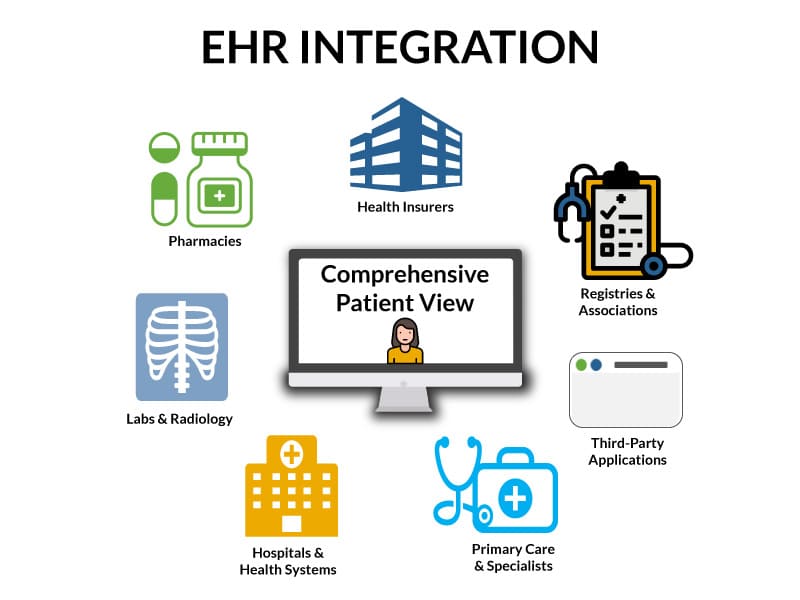
Electronic health record integration is the process of connecting and enabling seamless data exchange between various healthcare information systems, applications, and platforms. This goes far beyond basic EHR system connectivity—it encompasses comprehensive medical record system connectivity that unifies clinical workflows, administrative processes, and patient engagement tools, often incorporating personal health record software to enhance patient access and engagement.
EHR vs EMR: Critical Distinctions
| System Type | Scope | Key Features | Data Sharing |
|---|---|---|---|
| EMR (Electronic Medical Records) |
Single healthcare provider or organization | Medical history, diagnoses, medications, treatment plans | Limited – within organization only |
| EHR (Electronic Health Records) |
Multiple healthcare providers and organizations | Comprehensive data from labs, imaging centers, pharmacies, specialists | Extensive – across healthcare ecosystem |
The Current State of Healthcare EHR Interoperability
Adoption vs. Integration Reality
The healthcare industry has made remarkable progress in EHR adoption:
- 96% of non-federal acute care hospitals have adopted certified EHR technology Electronic Health Records Market Size, Share, Trends Report [2035]
- 78% of office-based physicians utilize certified EHR systems EHR Industry Statistics and Facts (2025)
- 83.40% of EHR systems are cloud and web-based as of 2024 Electronic Health Records Market Size to Hit USD 44.39 Bn by 2034
However, the interoperability challenge persists: Despite widespread adoption, only approximately 30% of healthcare providers have achieved full EHR interoperability, highlighting the massive opportunity for organizations that successfully implement comprehensive integration strategies.
Global Market Dynamics
The global electronic health records market is valued at $36 billion in 2024 and projected to reach $93 billion by 2035, representing a CAGR of 8.6%. This growth is driven by:
- Increasing demand for streamlined healthcare management
- Regulatory incentives for digital health records
- Integration of AI and data analytics in patient care
- Focus on value-based care models requiring comprehensive data access
Why Electronic Health Record Integration is Critical for Healthcare Success
1. Enhanced Patient Care and Clinical Outcomes
EHR integration directly impacts patient safety and care quality through:
- Real-time Clinical Decision Support: Approximately 80% of healthcare providers leverage EHR-based clinical decision support tools to enhance diagnostic accuracy and treatment planning. Electronic Health Records Market Size, Share, Trends Report [2035].
- Predictive Healthcare Analytics: EHR-integrated artificial intelligence algorithms demonstrate 95% accuracy in predicting patient disease progression, enabling proactive interventions.
- Reduced Medical Errors: Healthcare institutions using EHR data analytics report a 40% decrease in diagnostic errors compared to traditional paper-based record systems.
2. Substantial ROI and Cost Savings
The financial impact of effective hospital EHR integration is compelling:
- Revenue Optimization: Healthcare organizations with advanced data integration capabilities experience an average 25% increase in annual revenue through identification and optimization of care gaps and revenue opportunities.
- Operational Efficiency: Interoperability could save $30 billion annually in the U.S. healthcare system through reduced duplicate testing, improved care coordination, and streamlined administrative processes.
- Technology ROI: Healthcare organizations that effectively integrate analytics technologies achieve an average ROI of 147% on their analytics investments within three years, often partnering with specialized healthcare analytics companies to maximize data insights and clinical outcomes.
3. Operational Excellence and Workflow Optimization
Clinical data integration software enables:
- Comprehensive Data Access: Over 85% of EHRs offer seamless integration with laboratory systems, enabling real-time access to test results, while more than 70% of hospitals have integrated imaging and radiology results directly into EHRs.
- Administrative Efficiency: Administrative burdens account for up to 25% of healthcare costs Ahrq, making workflow automation through integration a significant opportunity for savings.
- Enhanced Care Coordination: More than 60% of healthcare organizations utilize secure messaging features within EHRs to enable secure communication between care team members and patients.
Key Benefits of Healthcare Data Integration Platforms
Clinical Benefits
- Holistic Patient View: Integration creates comprehensive patient profiles by aggregating data from multiple sources including laboratory results, imaging studies, pharmacy records, specialist consultations, and clinical notes.
- Evidence-Based Care: Predictive analytics applied to EHR data has led to a 20% reduction in hospital-acquired infections and 15% improvement in medication adherence among chronic disease patients.
- Care Continuity: Seamless information flow between care settings ensures continuity during transitions, reducing readmissions and improving patient outcomes.
Operational Benefits
- Workflow Automation: Integration eliminates manual data entry, reduces administrative burden, and enables staff to focus on patient care rather than data management.
- Resource Optimization: Better visibility into patient flow, bed utilization, and staff allocation enables improved resource management and capacity planning.
- Quality Reporting: Automated quality measures and regulatory reporting reduce compliance burden while ensuring accuracy.
Financial Benefits
- Value-Based Care Enablement: Integration provides the comprehensive data analytics required for successful participation in value-based care contracts and population health management.
- Cost Containment: Elimination of duplicate testing, reduced length of stay, and improved operational efficiency directly impact the bottom line.
- Revenue Cycle Enhancement: Streamlined billing processes leveraging EDI in healthcare protocols, improved documentation using standardized medical coding language, and better charge capture optimization increase revenue realization.
How to Implement EHR Integration: Step-by-Step Guide
| Phase & Timeline | Key Activities | Specific Tasks | Critical Success Factors |
|---|---|---|---|
| Phase 1 Pre-Implementation Assessment 2-4 weeks
|
Current System Audit | • Inventory all existing healthcare systems and applications • Document current data flows and integration points • Identify data silos and workflow inefficiencies • Assess API availability and technical constraints |
Stakeholder Buy-in
Thorough Analysis
Clear Requirements
|
| Stakeholder Analysis | • Engage clinical staff, IT teams, and administrative leadership • Document specific integration requirements by department • Define success metrics and performance indicators • Establish budget parameters and timeline expectations |
||
| Technical Assessment | • Evaluate network infrastructure and bandwidth capacity • Review security protocols and compliance requirements (HIPAA, GDPR) • Assess data mapping needs and standardization requirements • Identify training and change management needs |
||
| Phase 2 Vendor Selection & Strategic Planning 3-6 weeks
|
RFP & Vendor Evaluation | • Create detailed technical specifications and functional requirements • Evaluate vendors based on integration capabilities, security, and cost • Conduct proof-of-concept demonstrations with shortlisted vendors • Verify vendor compliance with healthcare regulations and standards |
Right Vendor Choice
Solid Architecture
Risk Mitigation
|
| Architecture Design | • Design technical architecture supporting HL7 FHIR standards • Plan API integration protocols and data exchange formats • Develop security framework including encryption and access controls • Create detailed project timeline and milestone tracking |
||
| Risk Assessment | • Identify potential technical, operational, and financial risks • Develop contingency plans for critical integration points • Plan phased implementation approach to minimize disruption • Establish rollback procedures and data backup protocols |
||
| Phase 3 Development & Integration Implementation 8-16 weeks
|
API Development | • Implement RESTful APIs following FHIR standards for interoperability • Configure data mapping between disparate systems and databases • Establish real-time data synchronization protocols • Test API performance and scalability under expected load |
Quality Assurance
Security First
User Training
Thorough Testing
|
| Security Implementation | • Deploy multi-layered security including AES-256 encryption • Implement role-based access controls and authentication protocols • Configure audit logging and monitoring systems • Ensure compliance with HIPAA, GDPR, and local regulations |
||
| Testing & QA | • Unit Testing: Verify individual integration components • Integration Testing: Test data flow between systems • User Acceptance Testing: Validate workflows with end users • Performance Testing: Ensure performance under peak loads |
||
| Staff Training | • Develop role-specific training programs for different user groups • Conduct hands-on training sessions with workflow simulations • Create user documentation and quick reference guides • Establish support channels for ongoing assistance |
||
| Phase 4 Go-Live & Optimization 4-8 weeks
|
Phased Deployment | • Start with pilot implementation in limited departments • Monitor system performance and user adoption closely • Gradually expand integration to additional departments • Maintain parallel systems during transition period |
Gradual Rollout
Performance Monitoring
ROI Tracking
|
| Performance Monitoring | • Track key performance indicators including system uptime and response times • Monitor data accuracy and integration success rates • Collect user feedback and identify optimization opportunities • Fine-tune system performance and resolve identified issues |
||
| Success Measurement | • Measure clinical outcomes including error reduction and efficiency gains • Track operational metrics such as workflow automation and time savings • Calculate financial ROI including cost savings and revenue improvements • Document lessons learned and best practices for future projects |
EHR Integration Costs and Pricing Models
Cost Breakdown by Organization Size
| Organization Size | Initial Implementation | Annual Maintenance | Total 3-Year Cost | Expected ROI |
|---|---|---|---|---|
| Small Practice (1-10 providers) |
$25,000 – $75,000 | $5,000 – $15,000 | $35,000 – $105,000 | 150% – 200% |
| Medium Practice (11-50 providers) |
$100,000 – $300,000 | $20,000 – $60,000 | $140,000 – $420,000 | 200% – 300% |
| Large Healthcare System (50+ providers) |
$500,000 – $2,000,000 | $100,000 – $400,000 | $800,000 – $3,200,000 | 250% – 400% |
Cost Factors and Considerations
Implementation Cost Components:
- Software Licensing: 30-40% of total implementation cost
- Custom Development: 25-35% for tailored integration solutions
- Hardware Infrastructure: 10-15% for servers and networking equipment
- Training & Change Management: 10-15% for staff preparation and adoption
- Project Management: 5-10% for coordination and oversight
Hidden Costs to Consider:
- Data Migration: Can add 20-30% to total project cost
- Downtime Costs: Potential revenue loss during transition periods
- Ongoing Support: Technical support beyond standard maintenance
- Compliance Auditing: Regular security and compliance assessments
- System Upgrades: Future enhancement and scalability requirements
ROI Calculation Framework
Cost Savings Calculation:
- Administrative Efficiency: Reduced manual data entry and processing time
- Duplicate Testing Elimination: Avoiding redundant laboratory and imaging studies
- Improved Care Coordination: Reduced readmissions and medical errors
- Revenue Cycle Optimization: Faster billing and improved documentation accuracy
ROI Formula:
ROI = (Annual Benefits - Annual Costs) / Total Implementation Cost × 100
Example for Medium Practice:
Annual Benefits: $180,000 (efficiency gains + error reduction)
Annual Costs: $40,000 (maintenance + support)
Implementation Cost: $200,000
ROI = ($180,000 - $40,000) / $200,000 × 100 = 70% annual ROITypical ROI Timeline:
- Year 1: 50-80% ROI as systems stabilize and staff adapt
- Year 2: 100-150% ROI with full workflow optimization
- Year 3+: 150-300% ROI through advanced analytics and optimization
EHR Integration Models and Technology Approaches
1. API-First Integration Architecture
Modern healthcare data integration platforms leverage RESTful APIs and FHIR standards to enable:
- Real-time Data Exchange: Immediate synchronization of patient information across all connected systems
- Scalable Infrastructure: Architecture that grows with organizational needs and technological advancement
- Standardized Connectivity: Consistent data formats and secure authentication protocols
2. Cloud-Based Integration Platforms
Cloud and web-based EHR systems dominate with 83.40% market share in 2024 Electronic Health Records Market Size to Hit USD 44.39 Bn by 2034, offering significant advantages:
- Reduced Infrastructure Costs: Minimal hardware requirements and lower maintenance overhead
- Automatic Updates: Continuous platform improvements and security enhancements
- Enhanced Disaster Recovery: Robust backup and recovery capabilities with geographic redundancy
3. Hybrid Integration Models
Many healthcare organizations adopt hybrid approaches combining on-premise and cloud solutions:
- Sensitive Data Control: Maintain critical data on-premise while leveraging cloud analytics and collaboration tools
- Gradual Transition: Enable phased migration strategies that minimize operational disruption
- Regulatory Flexibility: Adapt to changing compliance requirements while maintaining data sovereignty
Savvycom’s Expertise in Healthcare EHR Integration Solution
As a leading software development company with extensive experience in healthcare technology, Savvycom brings unique capabilities to the complex challenge of EHR system integration. Our approach combines deep technical expertise with practical understanding of healthcare workflows and regulatory requirements.
Comprehensive Healthcare Technology Solutions
Savvycom’s healthcare practice focuses on delivering end-to-end integration solutions that address the full spectrum of healthcare data management challenges:
- Custom EHR Development: Unlike off-the-shelf solutions, we develop tailored EHR systems that align precisely with organizational workflows and specific clinical requirements.
- International Compliance Expertise: Our global experience enables us to navigate complex regulatory environments including HIPAA, GDPR, and local healthcare data protection requirements across different markets.
- Scalable Architecture Design: We architect systems that accommodate growth, technological evolution, and changing regulatory landscapes while maintaining optimal performance and security.
Savvycom Case Study: Transforming Surgery Management Through Integration For Client

A premier healthcare institution partnered with Savvycom to enhance their surgery booking and communication systems through advanced EHR integration. This comprehensive project demonstrates our capability to transform complex healthcare workflows while maintaining the highest standards of patient care and data security.
Project Scope and Implementation:
- Pre-operative Integration: Unified patient data from multiple sources including medical history, lab results, imaging studies, and specialist consultations
- Intra-operative Coordination: Real-time data sharing between surgical teams, anesthesiologists, nursing staff, and support personnel
- Post-operative Continuity: Seamless transition of surgical data to recovery protocols and follow-up care management
Measurable Outcomes:
- Enhanced Workflow Efficiency: Streamlined surgical scheduling and resource allocation through integrated data access
- Improved Communication: Real-time information sharing eliminated communication delays and reduced potential for errors
- Better Patient Outcomes: Comprehensive data visibility enabled more informed clinical decision-making throughout the surgical journey
- Operational Excellence: Reduced administrative burden and improved resource utilization across the surgical department
Technical Innovation:
- API-Driven Architecture: Implementation of modern RESTful APIs ensuring scalable, maintainable integration
- Security Framework: Multi-layered security approach including encryption, access controls, and audit logging
- Regulatory Compliance: Full adherence to healthcare data protection regulations and industry best practices
Savvycom’s Competitive Advantages in Healthcare IT
- Custom Development Expertise: Our ability to create bespoke solutions tailored to specific organizational needs sets us apart from vendors offering only standardized products.
- Global Healthcare Experience: We understand the nuances of healthcare systems across different countries and regulatory environments, enabling successful international implementations.
- Cost-Effective Enterprise Solutions: Our development approach provides enterprise-grade functionality at a fraction of the cost of traditional healthcare IT vendors.
- Full-Stack Capabilities: From backend integration and database management to user interface design and mobile applications, we provide comprehensive technology solutions.
- Agile Implementation Methodology: Our proven project management approach ensures timely delivery while maintaining flexibility to adapt to changing requirements.
Implementation Best Practices for Healthcare Data Integration
1. Strategic Planning and Assessment
Comprehensive Needs Analysis: Conduct thorough evaluation of current systems, identify integration gaps, and define clear success metrics that align with organizational objectives.
Stakeholder Alignment: Engage clinical staff, IT teams, administrators, and executive leadership to ensure integration initiatives support broader strategic goals.
Risk Assessment: Identify potential challenges including technical constraints, regulatory requirements, and organizational change management needs.
2. Technology Architecture and Selection
Standards-Based Approach: Prioritize solutions supporting HL7 FHIR, SMART on FHIR, and other established interoperability standards to ensure long-term compatibility and flexibility.
Scalable Infrastructure: Design systems capable of accommodating growth in data volume, user base, and functional requirements over time.
Security-First Design: Implement comprehensive security measures from initial architecture through deployment and ongoing operations.
3. Change Management and Training
Clinical Workflow Integration: Ensure new systems enhance rather than disrupt existing clinical processes, incorporating feedback from end users throughout development.
Comprehensive Training Programs: Develop role-specific training that addresses both technical functionality and workflow changes.
Continuous Improvement: Establish feedback mechanisms and iterative enhancement processes to optimize system performance and user satisfaction.
4. Data Governance and Quality Management
Data Standardization: Implement consistent data formats, terminologies, and quality standards across all integrated systems.
Privacy and Security Protocols: Establish robust data governance frameworks ensuring compliance with healthcare regulations while enabling appropriate data sharing.
Performance Monitoring: Deploy comprehensive monitoring and analytics capabilities to track system performance, user adoption, and clinical outcomes.
Conclusion: Strategic Imperative for Healthcare Excellence
Electronic health record integration represents far more than a technological upgrade—it is a strategic imperative that determines healthcare organizations’ ability to deliver superior patient care while achieving operational excellence and financial sustainability in an increasingly complex and competitive environment.
The evidence is compelling: organizations that successfully implement comprehensive EHR integration strategies consistently outperform their peers across clinical, operational, and financial metrics. With the global EHR market projected to reach $93 billion by 2035 Electronic Health Records (EHR) Market Size | 4.32% CAGR and potential annual savings of $30 billion through improved interoperability, the business case for strategic integration is undeniable.
However, success requires more than technology implementation—it demands comprehensive change management, stakeholder engagement, and ongoing optimization. Healthcare organizations must approach EHR integration as a transformational journey that touches every aspect of their operations, from clinical workflows and patient engagement to financial management and regulatory compliance.
The path forward requires:
- Strategic Vision: Clear understanding of how integration supports broader organizational objectives
- Technology Excellence: Implementation of modern, standards-based solutions that provide scalability and future-readiness
- Change Management: Comprehensive approach to organizational transformation and user adoption
- Continuous Improvement: Ongoing optimization based on performance data and user feedback
- Partnership Approach: Collaboration with experienced technology partners who understand healthcare’s unique challenges and requirements
The future belongs to healthcare organizations that can seamlessly integrate data, workflows, and systems to create unified, patient-centered care experiences. By investing in comprehensive EHR integration strategies today, healthcare leaders position their organizations not just for immediate operational improvements, but for long-term success in the evolving healthcare landscape.
Ready to transform your healthcare organization through strategic EHR integration? The journey begins with understanding your unique requirements, developing a comprehensive integration strategy, and partnering with experienced healthcare technology specialists who can guide you through the complexities of modern healthcare data management. Contact healthcare integration experts to explore how custom EHR integration solutions can unlock your organization’s potential for clinical excellence and operational success.
For healthcare organizations seeking to implement or enhance their EHR integration capabilities, partnering with experienced development companies like Savvycom ensures access to proven expertise in healthcare technology, international compliance requirements, and scalable system architecture. Our comprehensive approach to healthcare data integration combines technical excellence with deep understanding of clinical workflows and regulatory environments, often incorporating innovative healthcare app ideas to enhance patient engagement and care delivery., enabling healthcare organizations to achieve their integration objectives while maintaining focus on their primary mission: delivering exceptional patient care.
2. How could integrating an EHR improve facility operations?
EHR integration eliminates duplicate data entry, reduces medical errors by 40%, and saves up to 25% in administrative costs. It enables real-time access to patient information across departments, streamlines billing processes, and improves care coordination. Staff can focus on patient care instead of searching for records across multiple systems.
3. What are the two types of EHR systems commonly used in healthcare?
The two main types are cloud-based EHRs (83% market share) offering lower costs and automatic updates, and on-premise EHRs providing greater data control and customization. Cloud systems are preferred by smaller practices, while large healthcare systems often choose hybrid models combining both approaches for optimal security and flexibility.
4. How much does EHR integration cost?
EHR integration costs vary by organization size: small practices ($25,000-$75,000), medium practices ($100,000-$300,000), and large healthcare systems ($500,000-$2,000,000). Annual maintenance adds 20-30% of initial cost. Most organizations see 150-400% ROI within three years through efficiency gains and cost savings.
5. What is the main difference between EHR and EMR?
EMRs (Electronic Medical Records) are digital charts used by single healthcare providers, containing basic patient information like diagnoses and medications. EHRs (Electronic Health Records) are comprehensive records shared across multiple providers, including data from labs, pharmacies, and specialists, enabling complete care coordination and better patient outcomes.


